Recently, the last patient completed Hepatitis C treatment with modern and effective direct-acting antivirals (DAAs) within the unique comprehensive three-year project implemented by the Alliance for Public Health “Scaling up Accessible and Effective HCV Treatment Through a Community–Based Treatment Model for Most Vulnerable Populations in Resource–Constrained Ukraine” (hereinafter – the Project).
Since April 2015, access to 1,907 courses of treatment within the Project was provided to the patients representing the key populations. 1,531 patients (80%) were people who inject drugs (PWID), 152 (8%) were partners of PWID; 69 (3.6%) – men who have sex with men; 82 (4.3%) – sex workers; 73 (3.8%) belonged to other groups, including 49 military servicemen involved in the armed conflict in the east of Ukraine.
1,400 patients (73.4%) were co-infected with HIV. The treatment success rate at the follow-up 12 weeks after the treatment completion was 95.1%. Out of all patients who received access to direct-acting antivirals, only 33 persons (1.7%) failed to complete their treatment due to various reasons.
Such a high success rate was reached by Alliance thanks to the design and further implementation of a unique model of community-based treatment and social support of patients from the key populations.
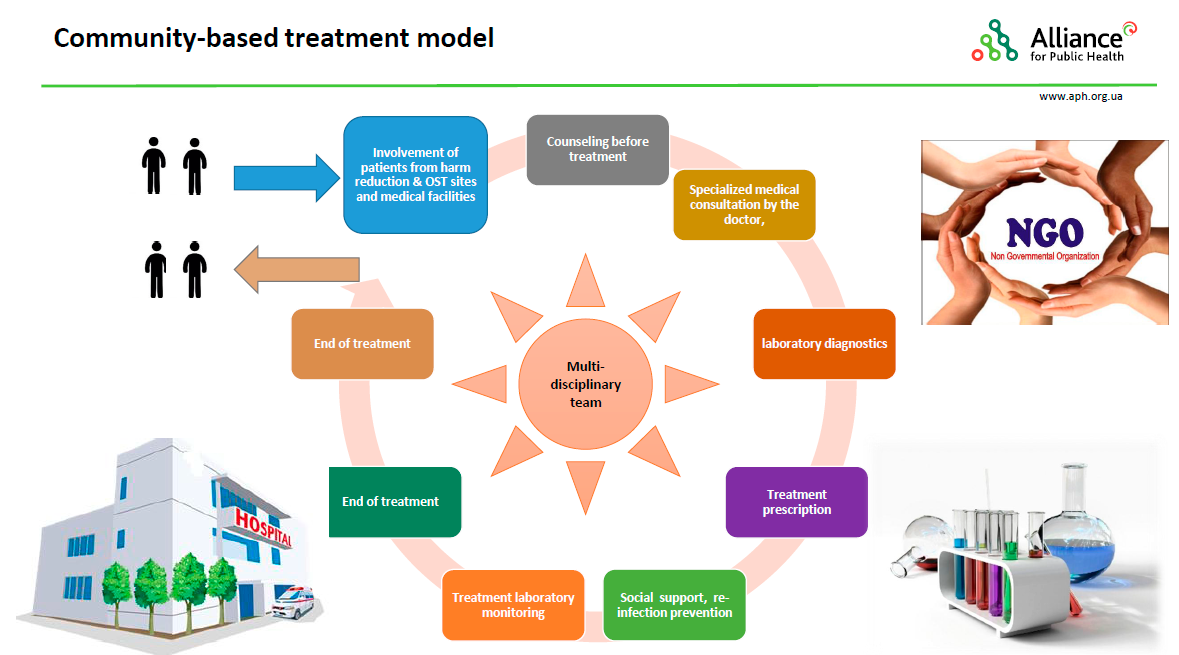
How did the model operate?
The first important step of the Project implementation was sharing accurate information about the Project conditions, eligibility criteria, advantages and opportunities with the key populations. This process was, first of all, facilitated by the social workers of local NGOs and community representatives who provided detailed information to potential participants of the Project and referred them to health facilities for consultations with doctors and further diagnostics. Each of the 25 health facilities involved into the Project organized multidisciplinary teams, each consisting of a doctor, a nurse and a social worker from one of the 19 local NGOs.
Second, Alliance offered a number of workshops for doctors and social workers on Hepatitis C treatment with direct-acting antivirals. The workshops also covered peculiarities of the patients’ psychosocial support in the course of treatment.
Coordinated decisions on the compliance with all eligibility criteria and final enrolment in the treatment program were taken by the multidisciplinary teams.
The criteria for patient enrolment and prioritization within the Project were as follows:
- PWID, OST patients, SW, MSM, military servicemen, human rights advocates for key populations;
- Fibrosis ≥ F2 (priority – F3, F4), including compensated cirrhosis or extrahepatic manifestations of the disease which are not contraindications for the Hepatitis C antiviral therapy.
 Further treatment of the patients was provided under the careful monitoring and supervision of the multidisciplinary team. Each member of the team worked with the patient according to his/her professional duties and functions.
Further treatment of the patients was provided under the careful monitoring and supervision of the multidisciplinary team. Each member of the team worked with the patient according to his/her professional duties and functions.
The infectious disease doctor ensured the selection of patients based on the clinical indications, prescribed the required laboratory and functional diagnostic procedures depending on the individual clinical situation and terms of the Project, defined the treatment regimen, ensured proper maintenance of the medical records, assessed the patient’s condition during the therapy, corrected any possible side effects or treatment complications, took measures to avoid unwanted interactions between the DAAs and other medications, controlled the intended use of medical drugs, etc.
The nurse ensured timely and proper dispensing of medical drugs to the patients, filled in medical records, referred the patient for laboratory diagnostics in line with the doctor’s prescriptions, and provided consultations to the patients on the possible side effects and treatment complications together with the social worker.

The social worker was usually the first to establish contact with the potential Project participant. He/she provided explanations and consultations to the members of key populations on the possibility of taking part in the Project, ensured referral of the clients with positive Hepatitis C rapid test results to health facilities for further diagnostics of Hepatitis C. Within the multidisciplinary team, the social worker took part in the selection process, provided psychosocial support to the patient in the course of treatment, offered consultative, psychological and practical help to the patient, formed the patient’s adherence to treatment, referred the patient to the doctor in case of any complications, monitored the dates of further visits and receipt of the medical drugs, maintained contact with the patient’s family members.
Alliance staff members heard a lot of grateful words addressed to the social workers from the Project participants. The doctors involved also appreciated high efficiency of the model implemented. The effective and well-coordinated efforts of the multidisciplinary teams allowed achieving an unprecedented level of adherence among the patients from among the key populations participating in the Project – 98.3%.
Alliance would like to take this opportunity to express its deepest respect to the doctors who were involved in the Project and a sincere gratitude to the staff of partner NGOs for their committed work with the patients!
The community-based Hepatitis C treatment model implemented by the Alliance is a crucial step to improve public health. This approach may be used as an evidence to strengthen the healthcare system and to inform the national Hepatitis C elimination policy.